 Background Ankylosing spondylitis is a rare autoimmune disease which includes inflammation of the spine and the sacroiliac joints. The sacroiliac joints are located at the base of the spine where the low back connects to the pelvis. Athletes typically affected are young males (15-30 years old) with regular low back pain and stiffness (more than three months) that is often worse in the morning, lasts longer than 30 minutes and improves with activity. While the exact cause of ankylosing spondylitis is unknown, there is an increased risk in people who have a gene that produces a protein called HLA-B27. Since it is mainly caused by genetics, having a family member with ankylosing spondylitis is a risk factor. A majority of cases are mild; however, ankylosing spondylitis has no cure and can become disabling. In the most advanced cases, the inflammation triggers extra bone growth, which can limit the motion of the back. Symptoms
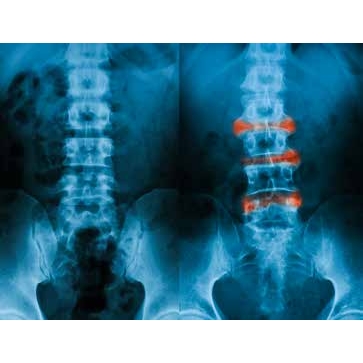
Sports Medicine Evaluation & Treatment Without the proper evaluation, ankylosing spondylitis may seem like a sports-related injury at first to those who are affected. The sports medicine physician might ask for a history of your symptoms and have you fill out a questionnaire. They would ask you to bend your neck and back to check your range of motion. The doctor would need to look at the skin on your neck, back, and hip. He or she would press on different areas to check for pain. The physician may order x-rays to look for changes in the bones or joints of the back and pelvis. Sometimes the doctor will order an MRI. This is an advanced imaging device that can show the signs of inflammation earlier in the disease, as well as rule out other injuries. You may be asked to get a blood test to check for markers of inflammation and/or to check for the presence of HLA-B27. Kids and adults may receive different treatments. Potential treatment options include:
Injury Prevention Although there are no current ways to avoid ankylosing spondylitis, earlier recognition, diagnosis, and treatment are very important to prevent the inflammation from causing longterm problems. Bringing down the inflammation reduces the severity of the symptoms, avoids the extra bone formation and ultimately improves performance in sports. Return to Play Symptoms such as pain and stiffness can limit sports participation, but exercise should still be encouraged. Many athletes experience significant improvement within one week of treatment. As symptoms improve, athletes may return to play as tolerated. AMSSM Member Authors References Category: Rheumatology , [Back] |

